ANTIMICROBIAL RESISTANCE, FACE OF ONE OF THE MAJOR PUBLIC HEALTH TRIALS!
What Is Antimicrobial Resistance?
Antimicrobial resistance takes place when germs like bacteria and fungi develop the capacity to setback the drugs deliberated to execute them, which means that germs instead of getting thwarted by the antibiotic, continues to breed causing innumerable health problems. Infections triggered by antibiotic-resistant germs are challenging, and many a times dreadful, to treat. In most cases, antibiotic-resistant infections require lengthy hospital stay, extra follow-up with the doctors, and expensive and toxic substitutes. In AMR the bacteria becomes resistant to the antibiotics intended to kill them.
Is It A Challenge In The Coming Times?
A detailed report from the WHO established that due to AMR, our reserves of operational antimicrobials are deteriorating swiftly. Similar to the living beings, microbes are sprouting for existence. AMR has been present even before the first ever antibiotic was revealed. AMR frequently advances due to discerning burden applied by antibiotic use, through genetic mutations or attainment of genetic material through plasmid transmission from an impervious bacterium.
AMR has been acknowledged as a worldwide health hazard with sombre health, political, and economic insinuations. The advancement made in modern medicine is under grave threat because of the advent of AMR. Annual deaths due to AMR are predicted to rise to 10 million worldwide by 2050. WHO stated that we not only advance AMR from medications, we also develop it by the wide-ranging use of antibiotics for livestock with the aim of averting their illness and intensify their productivity. So the illness and AMR transmit for us in food-borne disease.
Will India Face the Brunt too?
In emerging countries like India, current hospital and community centred data exhibited increase in burden of antimicrobial resistance. Research related to antimicrobial use, determinants and development of antimicrobial resistance, regional dissimilarity and interventional tactics bestowing to the current health care state in each country is a big trial. India lugs one of the major encumbrances of drug-resistant pathogens worldwide, comprising the maximum affliction of multidrug-resistant tuberculosis. Annually, more than 50,000 new-borns are assessed to die from sepsis due to pathogens resilient to first-line antibiotics.
While meticulous population burden approximations are not accessible, neonates and elderly are assumed to be worse affected. The spread of resistance is further aggravated by travel and population movement, making it easier for drug-resistant forms of a disease to spread to more people, and from one location to another. Self-medication is a popular practice in evolving countries where patients often get antimicrobials without prescription and through unfettered supply chains. The scene becomes even more complicated, where some patients pursue their treatment from traditional doctors who provide them with herbal permutations for the management of infections. These substances of unidentified configuration and effectiveness may augment pathogen fitness and contribute to the development of bacterial resistance.
The Economic Affect
Terrible public health setup, a heavy load of disease, and unfettered sales of antibiotics have backed the rapid rise in resilient infections in India. This has an enormous socio-economic effect due to deaths and amplified costs due to extended stay in hospital, additional and repetitive laboratory investigations, and loss of work for treating resistant bacterial infections. The impacts of AMR on the Indian economy could be huge and unforgiving.
Steps To Control The Worms Out Of The Can
Recommended approaches by WHO are listed below:
Augmented association amongst government, nongovernmental organizations, professional groups and international agencies:
- New networks that undertake surveillance of antimicrobial use and AMR.
- International methods for control of fake antimicrobials.
- Impetuses for the research and development of new drugs and vaccines.
- Finding new and strengthening prevailing programmes, to contain AMR.
What Can Be Done At Our Level?
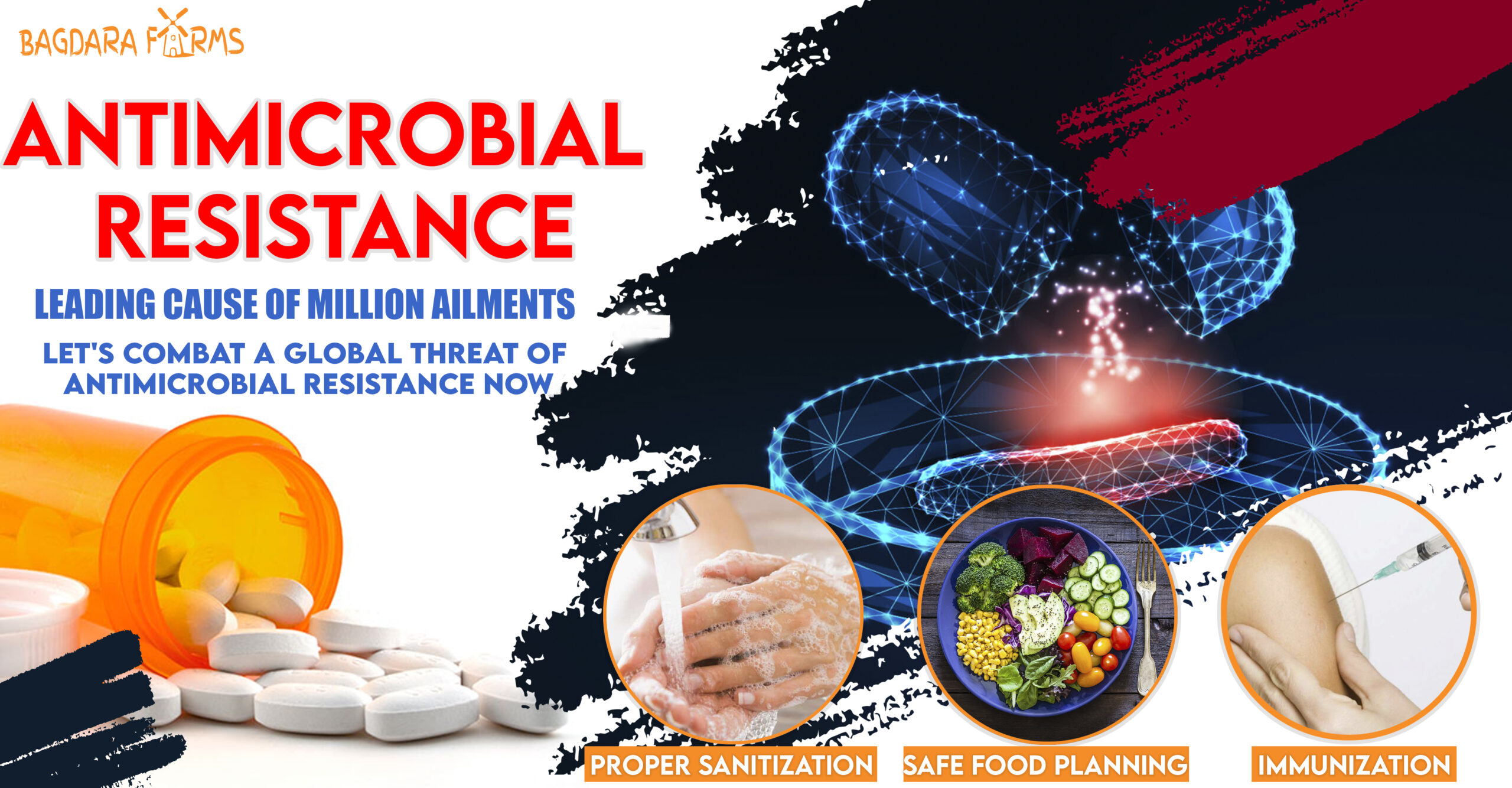
At our level there are many ways that drug-resistant infections can be forbidden by:
Immunization, safe food planning, hand washing, and using antibiotics, as told by the doctor and only when important. Preventing infections also averts the spread of resistant bacteria.
Let’s All Do It Together!
Unless we all work together now, regular infections could once again kill us, because they cannot be treated by antibiotics. Common operations such as hip replacements or organ transplants could become deadly because of the risk of infection. AMR is severe and one of the major causes of sickness and mortality; it makes it hard for a patient who has AMR to obtain suitable treatment whenever in need. The cost of dealing with AMR increases for the patients who develop antimicrobial resistance for many antibiotics. The spread of resistance is further aggravated by travel and population movement, making it easier for drug-resistant forms of a disease to spread to more people, and from one location to another.
Antimicrobial resistance (AMR) lingers to pose a significant public health problem in terms of mortality and economic loss. Efforts to combat AMR have been initiated by the Indian health authorities but are still at preliminary stages. The National Health Mission of India started the Swachh Bharat Abhiyan or the Clean India Mission to improve the basic hygiene and sanitation in all spheres of life and it is our duty to hold it up in letter and spirit.